GENDER: Male
AGE: 68 years old
DEVICE: coraForce™
PHYSICIAN: Vinod Nair, MD
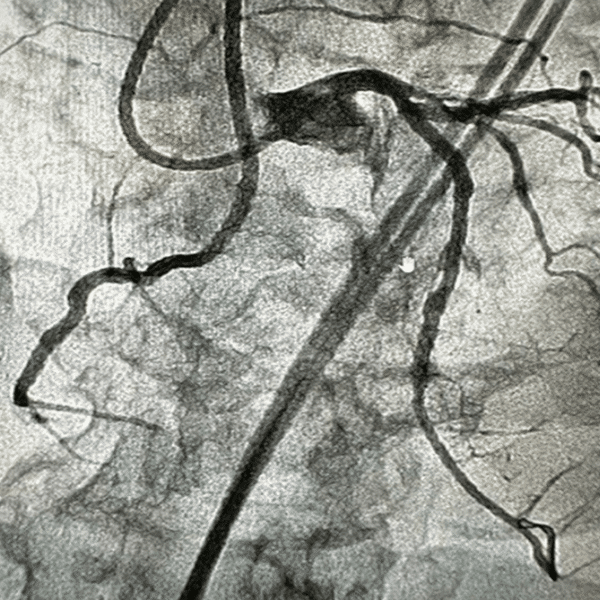
A 68-year-old male with a history of exertional chest pain (CCS III), despite optimal antianginal therapy and dyslipidemia. Diagnostic imaging showed a medium, partially reversible perfusion defect of severe intensity in the inferior region of the heart.
GENDER: Female
AGE: 77 years old
DEVICE: coraForce™
PHYSICIAN: Rajiv Tayal, MD, MPH, FACC, FSCAI, RPVI
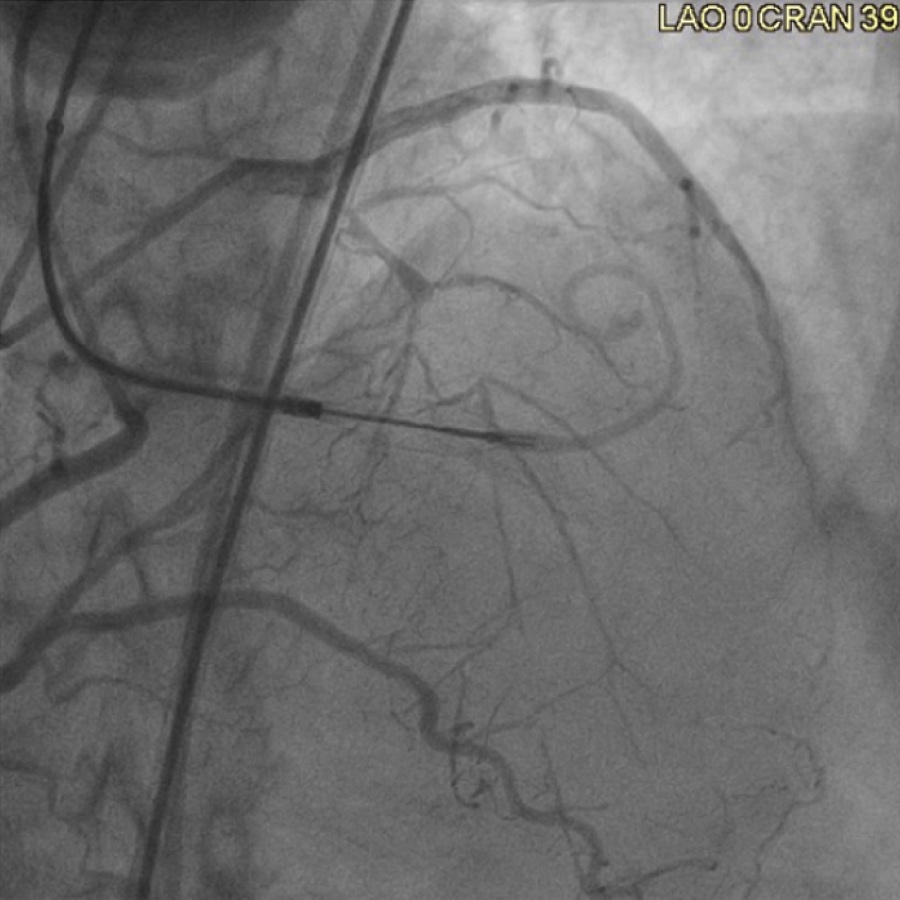
A 77-year-old women with a history of hypertension, dyslipidemia, diabetes, morbid obesity, and left bundle branch block was referred to our facility. The patient had worsening dyspnea on exertion and had failed PCI of a chronic total occlusion (CTO) at another facility. An abnormal nuclear stress test showed moderate reversible ischemia and newly reduced left ventricular ejection fraction (LVEF) of 30%–35%. The CTO measured 20 mm on angiography, which showed a blunt proximal cap at the diagonal and septal branches in the mid left anterior descending (LAD) artery. There was also a new occlusion in the dominant left circumflex (LCX) artery, which had 90% stenosis.
GENDER: Male
AGE: 69 years old
DEVICE: coraFlex™
PHYSICIAN: Lorenzo Azzalini, MD, PhD, MSc, FACC, FSCAI
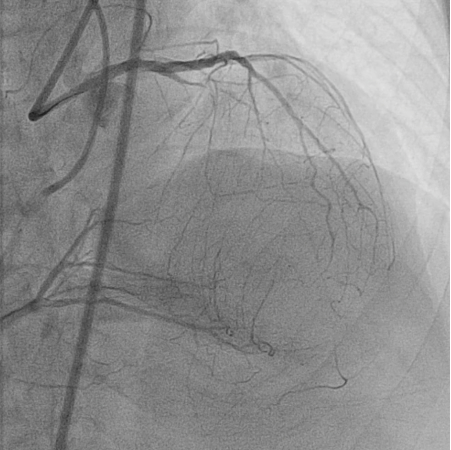
A 69-year-old man presented with fatigue and dyspnea on moderate exercise. Echocardiogram showed a left ventricular ejection fraction (LVEF) of 25%. Dual angiography revealed a proximal chronic total occlusion (CTO) in the proximal left anterior descending (LAD) artery, with an ambiguous proximal cap owing to a side branch. The occlusion was ~10mm with mild calcification. Septal collaterals from the right coronary artery (RCA) were also apparent. The J-CTO score was 1.