Revolutionary Below-the-Knee (BTK) Treatment for Chronic Limb-Threatening Ischemia (CLTI) in Conjunction with Drug-Coated Balloon (DCB)
SPUR RETRIEVABLE SCAFFOLD THERAPY
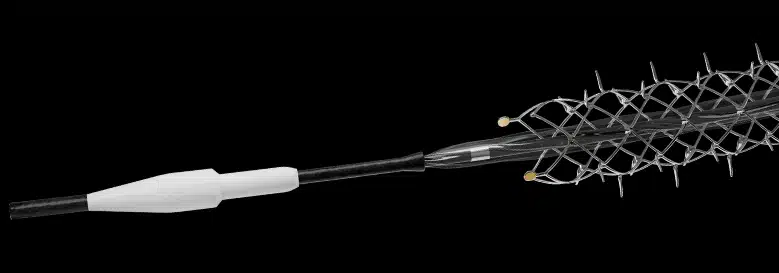
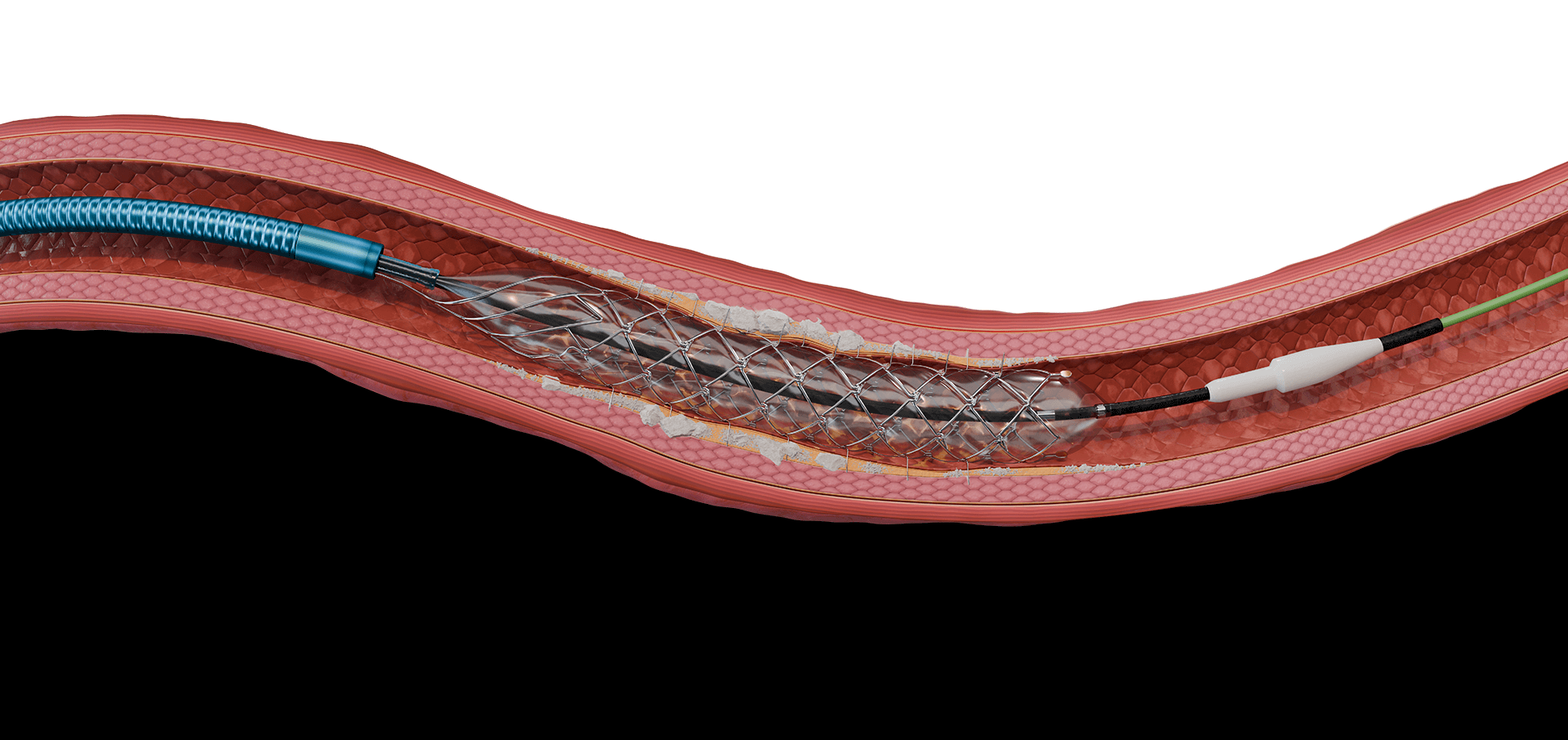
A self-expanding scaffold with integrated dilation balloon catheter designed for controlled penetration and lesion preparation through a series of radially expandable spikes. Spur creates channels that modify the lesion morphology, decreasing the recoil effect and changing vessel compliance. Channels optimize drug uptake when used with a commercially available drug-coated balloon (DCB).
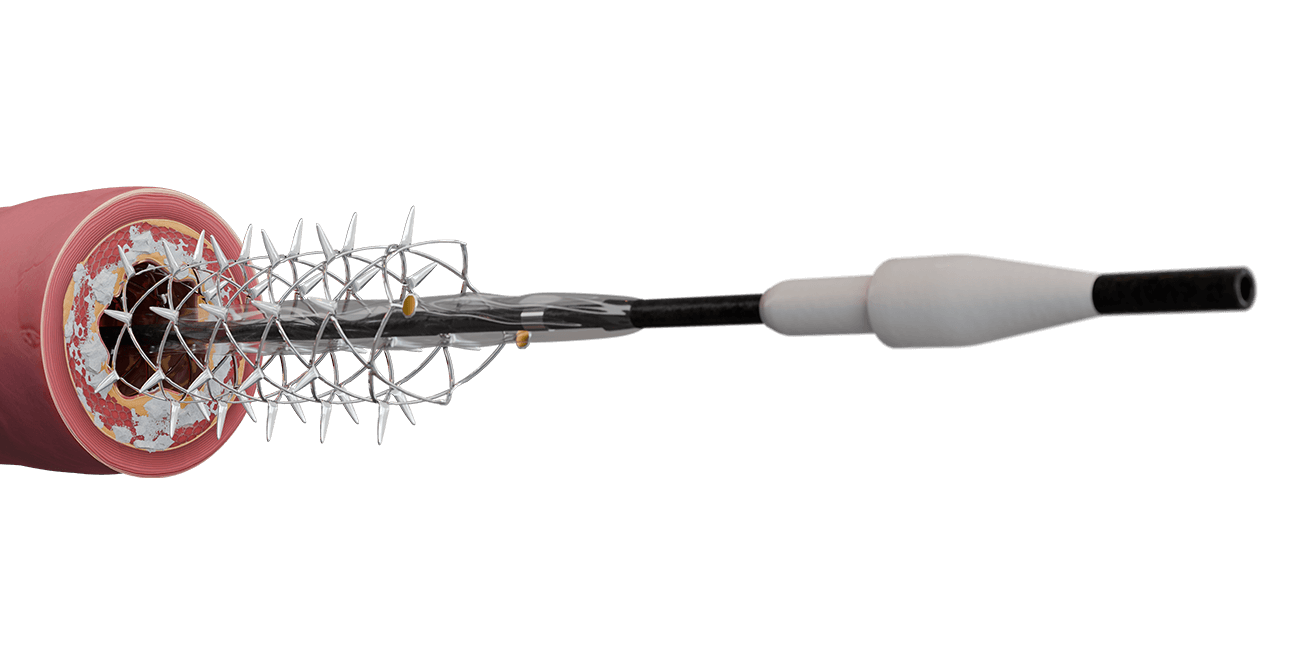
Retractable shaft—6F sheath compatible
Spikes optimized for controlled penetration and lesion preparation
Integrated balloon system for improved conformability
Radiopaque markers for visibility
.014″ guidewire
Familiar pin-and-pull Spur deployment system
3.0mm and 4.0mm device diameters conform to vessel anatomy
RST Mechanism of Action
- Track Spur system to lesion site and deploy using pin-and-pull method.
- Inflate integrated balloon in a controlled fashion.
RADIAL SPIKES PENETRATE THE VESSEL WALL AND CREATE CHANNELS DESIGNED TO:
- modify lesion morphology to change vessel compliance and reduce vessel recoil, and
- enhance drug absorption.
- Scaffold provides temporary supportive structure.
- Deflate the balloon and recapture the Spur system.
- Treat lesion with any commercially available DCB.
- Durable safety and efficacy outcomes leaving nothing behind.
FAMILIAR PIN-AND-PULL SPUR DEPLOYMENT SYSTEM

Clinically Proven
MAXIMIZING BTK TREATMENT OUTCOMES WITHOUT COMPROMISING ON SAFETY
DEEPER OUS
Prospective, multicenter, single-arm, performance goal comparator
12-MONTH RESULTS¹
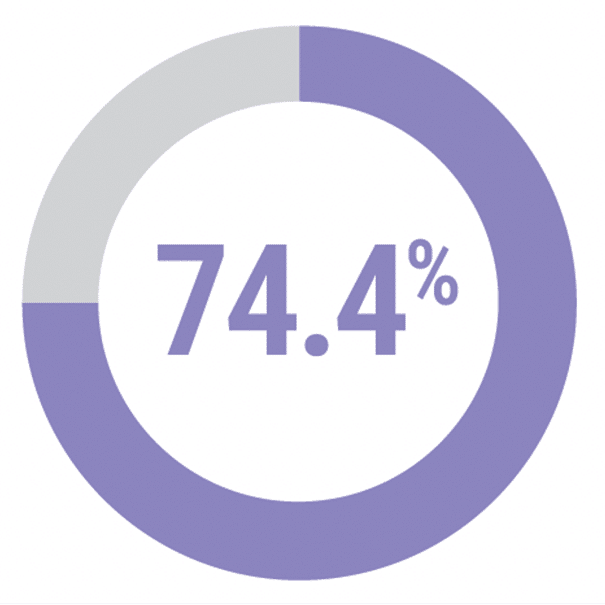
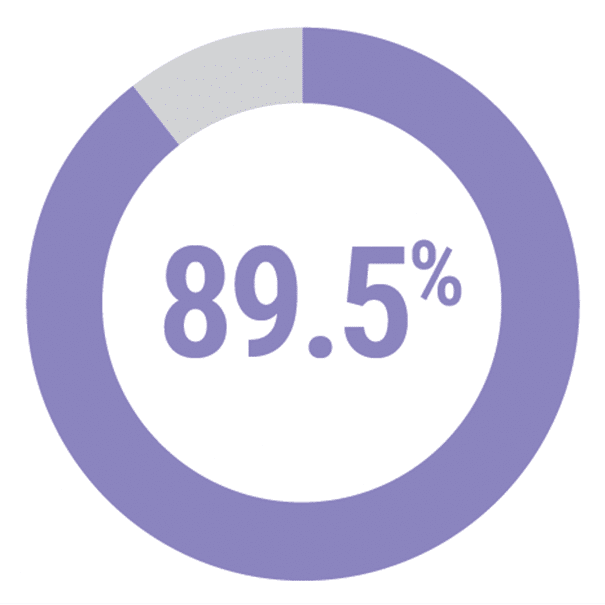
Patency of
lesions (DUS)
Freedom from
MALE
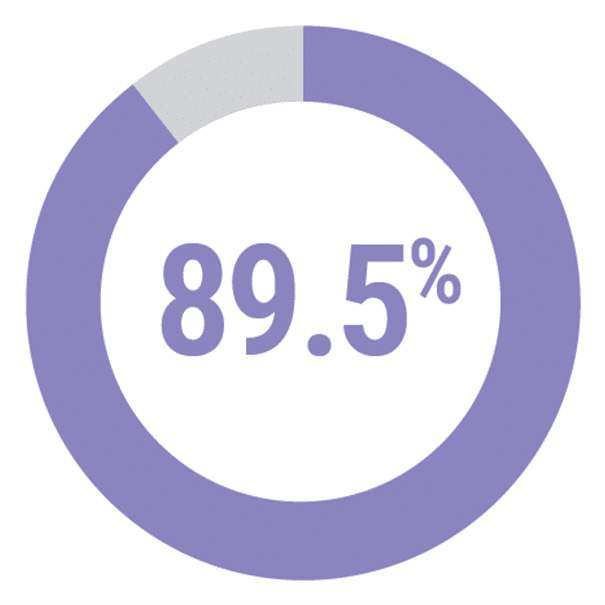
Freedom from
CD-TLR
RUTHERFORD SCORE IMPROVEMENT
58.4%
improvement in mean Rutherford score from the baseline
WOUND SIZE REDUCTION
63.1%
Reduction
STUDY DEVICES
Spur + paclitaxel-coated DCB*
STUDY SIZE
107 patients enrolled
10 centers (EU + NZ)
BASELINE LESION
CHARACTERISTICS
21% total occlusions
21% moderately/severely calcified lesions
92.7mm (60-240mm)
mean Spur-treated length (range)
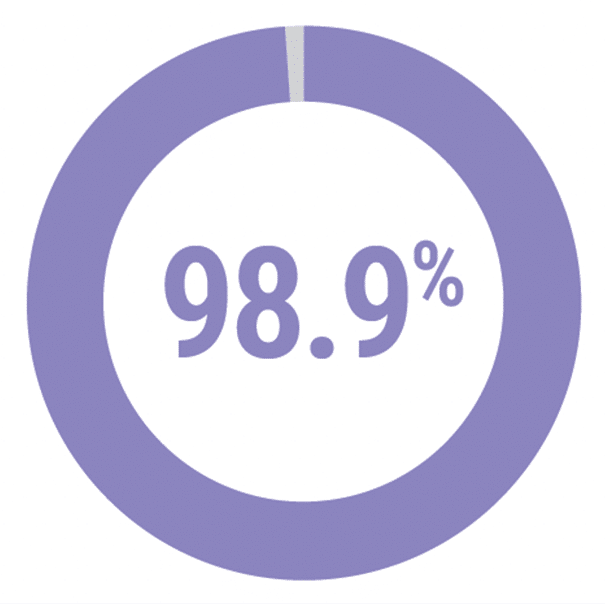
DEEPER LIMUS
Prospective, single-center, pilot, single arm
12-MONTH RESULTS²
Patency of
lesions (DUS)
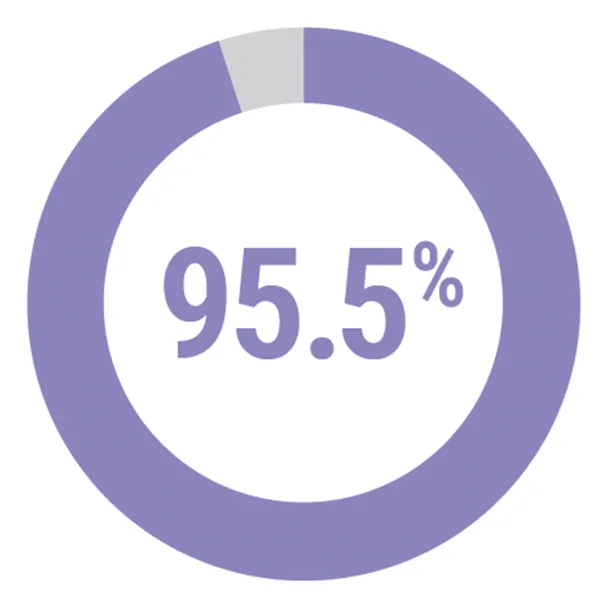
Freedom from
MALE
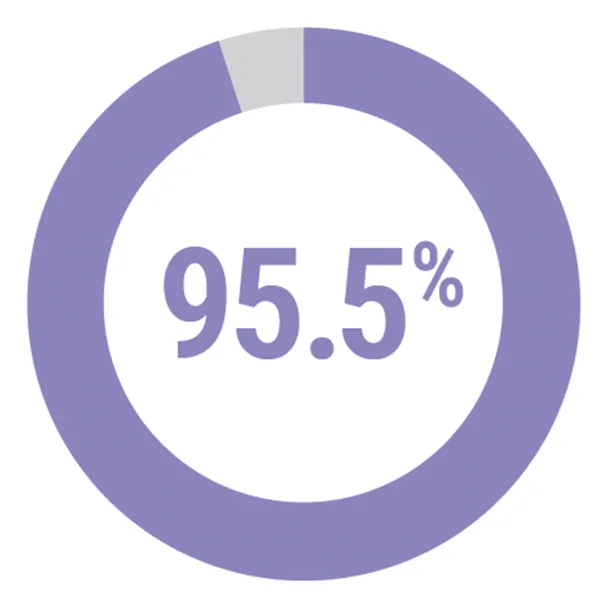
Freedom from
CD-TLR
RUTHERFORD SCORE IMPROVEMENT
68.2%
subjects improved to Rutherford classification 0
WOUND SIZE REDUCTION
54.0%
Reduction
STUDY DEVICES
Spur + sirolimus-coated DCB**
STUDY SIZE
26 patients enrolled
1 center (Austria)
BASELINE LESION
CHARACTERISTICS
37% total occlusions
97mm (60-210mm)
mean Spur-treated length (range)
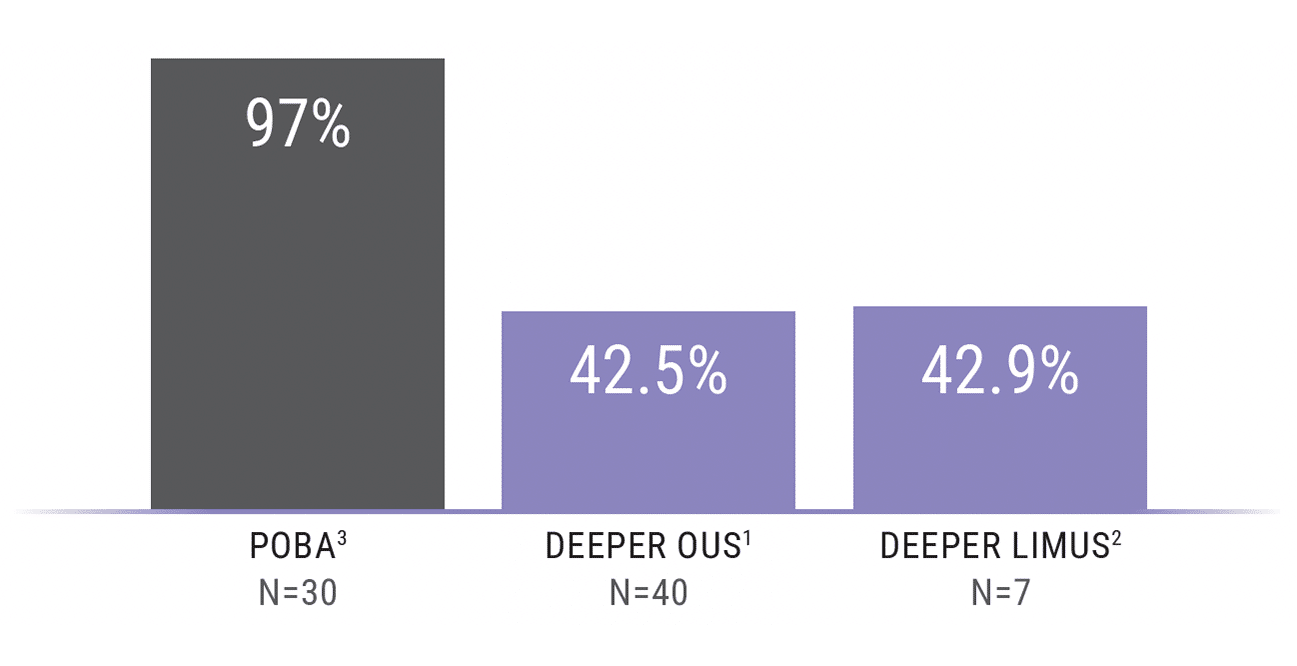
VESSEL RECOIL
Occurrence of vessel recoil
Defined as lumen compromise
≥10% at 15 minutes post
Spur treatment
Clinical Validation
| 23 patients; Dominican Republic |
| Prospective, single-center, first-in-human, single-arm |
| Spur + Lutonix DCB |
| Mean Spur Treated Length: 113mm (67.2-158.8) |
|
Abbreviations: DCB, drug-coated balloon; DUS, duplex ultrasound; MALE, major adverse limb event; POD, perioperative death; PP, primary patency.
| 107 patients: Europe, New Zealand |
| Prospective, multicenter, single-arm, performance goal comparator |
| Spur + paclitaxel DCB |
| Mean Spur Treated Length: 92.7mm (60-240) |
|
| Occurrence of vessel recoil: <43% (defined as lumen compromise ≥10% at 15 min. post Spur treatment) |
Abbreviations: DCB, drug-coated balloon; DUS, duplex ultrasound; MALE, major adverse limb event; POD, perioperative death; PP, primary patency.
| 26 patients; Austria |
| Prospective, single-center, pilot, single-arm |
| Spur + sirolimus DCB |
| Mean Spur Treated Length: 97mm (60-210) |
|
| Occurrence of vessel recoil: <43% (defined as lumen compromise ≥10% at 15 min. post Spur treatment) |
Abbreviations: DCB, drug-coated balloon; DUS, duplex ultrasound; MALE, major adverse limb event; POD, perioperative death; PP, primary patency.
DEEPER
| 23 patients; Dominican Republic |
| Prospective, single-center, first-in-human, single-arm |
| Spur + Lutonix DCB |
| Mean Spur Treated Length: 113mm (67.2-158.8) |
|
COMPLETED
Abbreviations: DCB, drug-coated balloon; DUS, duplex ultrasound; MALE, major adverse limb event; POD, perioperative death; PP, primary patency.
DEEPER OUS
| 107 patients: Europe, New Zealand |
| Prospective, multicenter, single-arm, performance goal comparator |
| Spur + paclitaxel DCB |
| Mean Spur Treated Length: 92.7mm (60-240) |
|
| Occurrence of vessel recoil: <43% (defined as lumen compromise ≥10% at 15 min. post Spur treatment) |
COMPLETED
Abbreviations: DCB, drug-coated balloon; DUS, duplex ultrasound; MALE, major adverse limb event; POD, perioperative death; PP, primary patency.
DEEPER LIMUS
| 26 patients; Austria |
| Prospective, single-center, pilot, single-arm |
| Spur + sirolimus DCB |
| Mean Spur Treated Length: 97mm (60-210) |
|
| Occurrence of vessel recoil: <43% (defined as lumen compromise ≥10% at 15 min. post Spur treatment) |
COMPLETED
Abbreviations: DCB, drug-coated balloon; DUS, duplex ultrasound; MALE, major adverse limb event; POD, perioperative death; PP, primary patency.

Reference Vessel Diameter (mm)
2.5–3.5
3.5–4.5
Model
BSPUR365135CE / BSPUR365150CE
BSPUR460135CE / BSPUR460150CE
Device Diameter (mm)
3.0
4.0
Device Length (mm)
65
60
Catheter Effective Length (cm)
135 / 150
135 / 150
Catheter OD (in/F/mm)
.074/5.6/1.88
.074/5.6/1.88
Guidewire Compatibility (in)
.014
.014
Sheath Compatibility (F/mm)
6/2.0
6/2.0
Balloon Diameter @ NP 6atm (mm)
3.00
4.02
Balloon Diameter @ RBP 12atm (mm)
3.20
4.23
Hydrophilic Coating—Distal (cm)
30
30
References
1. Data on file for DEEPER OUS clinical trial (NCT03807531)
2. Data on file for DEEPER LIMUS clinical trial (NCT04162418)
3. Baumann et al. (2014). Early recoil after balloon angioplasty of tibial artery obstructions in patients with critical limb ischemia. Journal of Endovascular Therapy, 2014(21): 44–51
* any commercially available DCB
** Concept Medical™ MagicTouch™ PTA
Indications, Safety, & Warnings
CAUTION: This device is restricted to use by or on the order of a physician. Refer to the Instructions for Use for a complete listing of the Indications, Contraindications, Warnings, Precautions, Adverse Events, and Procedural Steps.
Intended Use
The Spur is intended to treat de novo or restenotic lesions in the infrapopliteal arteries to prepare the vessel for treatment with a commercially available drug coated balloon to enhance drug absorption.
Indications for Use
The Spur is indicated for treatment of de novo or restenotic infrapopliteal lesions, with reference vessel diameters ranging from 2.5 – 4.5mm, prior to treatment with a commercially available drug coated balloon.
Contraindications
The Spur is not intended for use in coronary and cerebral vasculature.
Warnings
- Do not use the device past the expiration date on the label. Use of expired products may result in patient injury.
- Inspect the device packaging prior to use. Do not use the device if the device packaging has been damaged or if sterility has been compromised. Damaged product could result in patient injury.
- Ensure the Spur is used with appropriately sized ancillary devices as listed in the section below. Failure to do so could result in inadequate device performance or patient injury.
- Remove excess slack from the catheter (outside of the patient) to ensure the Spur is recaptured appropriately.
- If an inability to inflate or maintain balloon pressure occurs, remove the device and use a new one.
- Do not use excessive force or torque (more than 1 full turn) on the catheter as this could result in damage to the device and result in patient injury.
Precautions
- This device should only be used by physicians experienced in interventional vascular procedures.
- The system is intended for single (one) use only. DO NOT re-sterilize and/or reuse.
- Inflate the balloon according to the balloon compliance chart. Balloon pressure should not exceed the rated burst pressure (RBP).
- Use only the recommended contrast medium to inflate the balloon to ensure adequate delivery.
- Perform all device manipulations under adequate fluoroscopy.
- Do not advance or retract the catheter unless the balloon is fully deflated under vacuum. If resistance is met, determine the cause of the resistance before proceeding.
- Do not attempt to straighten a catheter if the shaft has become bent or kinked. Instead prepare a new catheter.
- During the procedure appropriate anticoagulant therapy must be provided to the patient as needed. Antiplatelet therapy should be prescribed post procedure in accordance with the treating physicians routine practice for endovascular procedures.
- Precautions should be taken when handling the device after exposure to patient, e.g. contact with blood. Used products are considered biohazardous material and should be disposed of properly as per hospital procedure.
Adverse Events
The following events are potential adverse effects associated with standard catheter-based peripheral interventions:
- Anemia;
- Edema;
- Hematoma;
- Peripheral arterial reocclusion;
- Peripheral artery dissection;
- Peripheral artery recoil;
- Pseudoaneurysm;
- Radiocontrast nephropathy;
- Vascular access site pseudoaneurysm;
- Vasospasm;
- Vessel perforation;
- Occlusion;
- Sepsis/Infection;
- Additional intervention;
- Short term hemodynamic deterioration;
- Stroke;
- Death;
- Heart attack;
- Vessel rupture;
- Hemorrhage;
- Pain or tenderness;
- Embolization;
- Arrhythmia;
- Shock.
©2024 Reflow Medical, Inc. All rights reserved. Reflow Medical, Spur and The Pulse of Medical Ingenuity are registered trademarks or trademarks of Reflow Medical, Inc. This device is restricted to use by or on the order of a physician. Refer to the Instructions for Use for a complete listing of the Indications, Contraindications, Warnings, Precautions, Adverse Events, and Procedural Steps.

QUESTIONS?
TALK TO A REFLOW PRO.
For more information, please send us your question or request today.
A Reflow pro will get back to you.